Outcome Data
The upper GI unit has carefully chosen a number of outcome and quality measures that will be reported on annually and freely available. These include information on referral patterns, performance against national surgical targets, specific procedural data and research and publication outputs.
The information in this section summarizes the upper gastrointestinal units experience with the major surgical procedures (gastro-oesophageal resections, pancreatic resections, hepatic resections and cholecystectomy) that it carries out on an annual basis. The information is taken from the Department of Surgery audit that is updated and reviewed weekly. Information is presented on anastomotic leak rates for gastro-oesophageal surgery, bile leak rates for hepatic resection and cholecystectomy, pancreatic leak rates for pancreatic resection and 30 and 90 day mortality is presented for all procedures. The leak rates are derived from audit codes specifically coding for these when they are diagnosed and also include patients in whom an intra-abdominal collection was diagnosed as a collection is often a sign of a leak. All complications are those graded Clavien-Dindo1 grade 3 or above meaning they were significant and required specific treatment.
All adverse outcomes are reviewed in the weekly Department of Surgery morbidity and mortality meeting as well as a formal quarterly in depth review by the upper gastrointestinal multidisciplinary team.
1.Dindo D; Demartines N; Clavian P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-213
| Procedures | Leaks (CD≥III) | 30 Day Mortality | 90 Day Mortality | |
| 2014 | 27 | 4 | 1 | 2 |
| 2015 | 23 | - | 1 | 3 |
| 2016 | 24 | 2 | - | 1 |
| 2017 | 35 | 3 | - | 1 |
| 2018 | 35 | 3 | - | - |
| 2019 | 36 | 4 | 1 | 2 |
| 2020 | 32 | 0 | - | - |
| 2021 | 48 | 4 | 0 | 1 |
| 2022 | 57 | 3 | 0 | 1 |
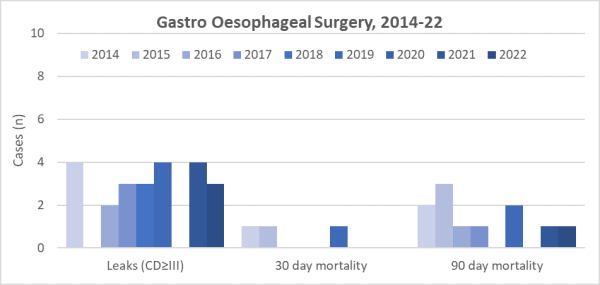
Commentary
- There have been 316 Gastro Oesophageal Surgery cases between 2014-22.
- In total, 7% (n= 23) had an intra-abdominal collection or anastomotic Leak (CD ≥III), 30 day post-op mortality was 1% and 90 day mortality was 3%.
Intra-abdominal collection, Bile Leak
| Procedures | Leaks (CD≥III) | 30 Day Mortality | 90 Day Mortality | |
| 2014 | 38 | 2 | - | 2 |
| 2015 | 42 | 1 | 2 | 3 |
| 2016 | 38 | 2 | - | - |
| 2017 | 42 | 5 | 3 | 3 |
| 2018 | 31 | - | 1 | 1 |
| 2019 | 44 | 2 | 4 | 5 |
| 2020 | 51 | 1 | 1 | 1 |
| 2021 | 47 | 3 | 1 | 1 |
| 2022 | 54 | 2 | 0 | 0 |
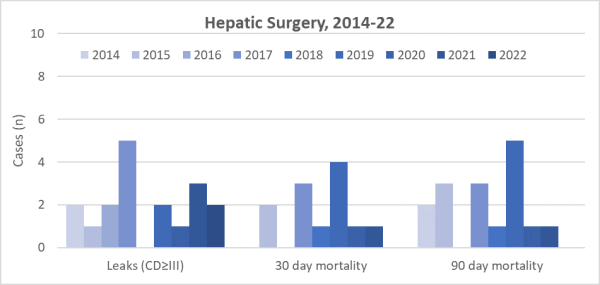
Commentary
- There have been 387 Hepatic Surgery cases between 2014-22.
- In total, 5% (n= 18) had an intra-abdominal collection or bile Leak (CD ≥III), 30 day post-op mortality was 3% and 90 day mortality was 4%.
| Procedures | Leaks (CD≥III) | 30 Day Mortality | 90 Day Mortality | |
| 2014 | 20 | 4 | 1 | 1 |
| 2015 | 22 | - | 2 | 3 |
| 2016 | 19 | - | 2 | 2 |
| 2017 | 27 | 1 | 1 | 1 |
| 2018 | 23 | - | - | 2 |
| 2019 | 13 | - | - | - |
| 2020 | 24 | 0 | - | - |
| 2021 | 37 | 1 | - | - |
| 2022 | 36 | 1 | 0 | 1 |
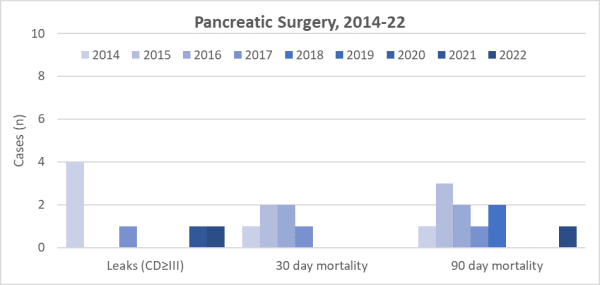
Commentary
- There were 218 Pancreatic Surgery cases between 2014-22.
- In total, 3% (n= 7) had a pancreatic leak (CD≥III), 30 day post-op mortality was 3% and 90 day mortality was 5%.
| Procedures | Leaks (CD≥III) | 30 Day Mortality | 90 Day Mortality | |
| 2014 | 594 | 8 | 1 | 3 |
| 2015 | 534 | 7 | 4 | 4 |
| 2016 | 572 | 5 | 1 | 1 |
| 2017 | 651 | 6 | - | 1 |
| 2018 | 609 | 5 | - | - |
| 2019 | 649 | 4 | - | - |
| 2020 | 659 | 3 | 1 | 2 |
| 2021 | 681 | 10 | - | 1 |
| 2022 | 825 | 8 | 2 | 2 |
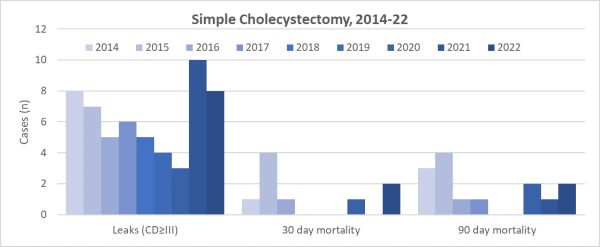
Commentary
- There were 5,774 Simple Cholecystectomy cases between 2014-22.
- In total 1% (n=56) had an intra-abdominal collection or bile leak (CD ≥III), 30 day post-op mortality was 0.2% and 90 day mortality was 0.2%.





