 As part of your treatment journey, you may be requried to complete a comprehensive assessment. This may involve questionnaires to assess pelvic function and continance, pain, occupational and sexual function, quality of life, and psychological distress.
As part of your treatment journey, you may be requried to complete a comprehensive assessment. This may involve questionnaires to assess pelvic function and continance, pain, occupational and sexual function, quality of life, and psychological distress.
Additional tests may be performed such as bladder function tests (urodynamics), examination under general anaesthetic, cystoscopy (a camera to look inside the bladder), specialised ultrasound and/or magnetic resonance imaging (MRI). The decision about which tests to perform will be made by the clinical team in discusion with you, and will depend on your individual circumstances.







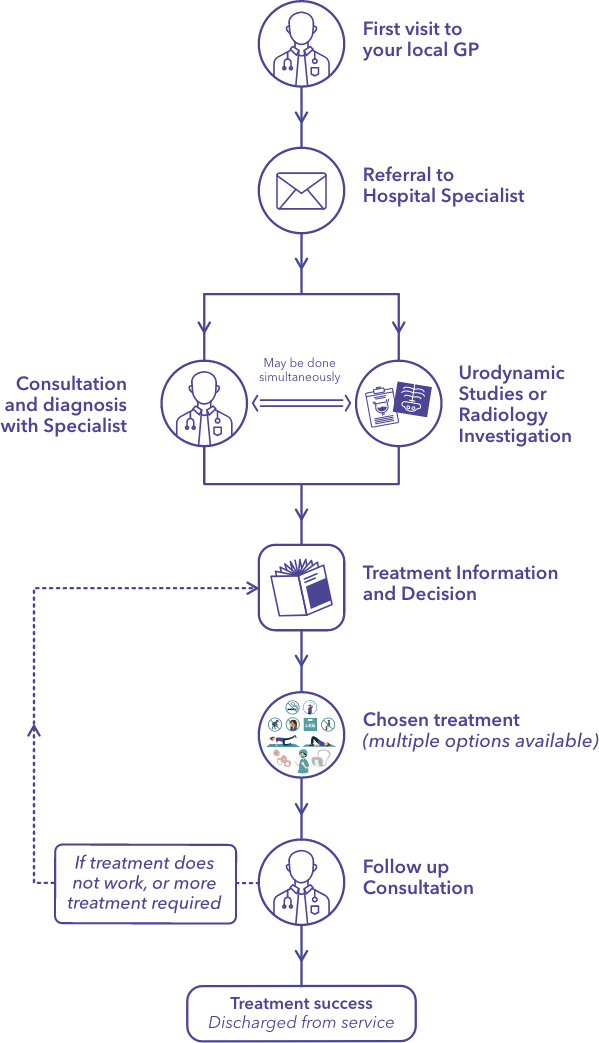
 You will likely be referred to us by your GP. Here is what you can do to prepare for your first appointment with us:
You will likely be referred to us by your GP. Here is what you can do to prepare for your first appointment with us: As part of your treatment journey, you may be requried to complete a comprehensive assessment. This may involve questionnaires to assess pelvic function and continance, pain, occupational and sexual function, quality of life, and psychological distress.
As part of your treatment journey, you may be requried to complete a comprehensive assessment. This may involve questionnaires to assess pelvic function and continance, pain, occupational and sexual function, quality of life, and psychological distress. We have a team of Booking Clerks, Peri-operative Coordinators and Clinical Nurse Specialists who oversee your journey with us.
We have a team of Booking Clerks, Peri-operative Coordinators and Clinical Nurse Specialists who oversee your journey with us.





 You may find it helpful to take a family member or friend for support when discussing your options and the next steps with your doctor.
You may find it helpful to take a family member or friend for support when discussing your options and the next steps with your doctor.